You have no items in your cart.

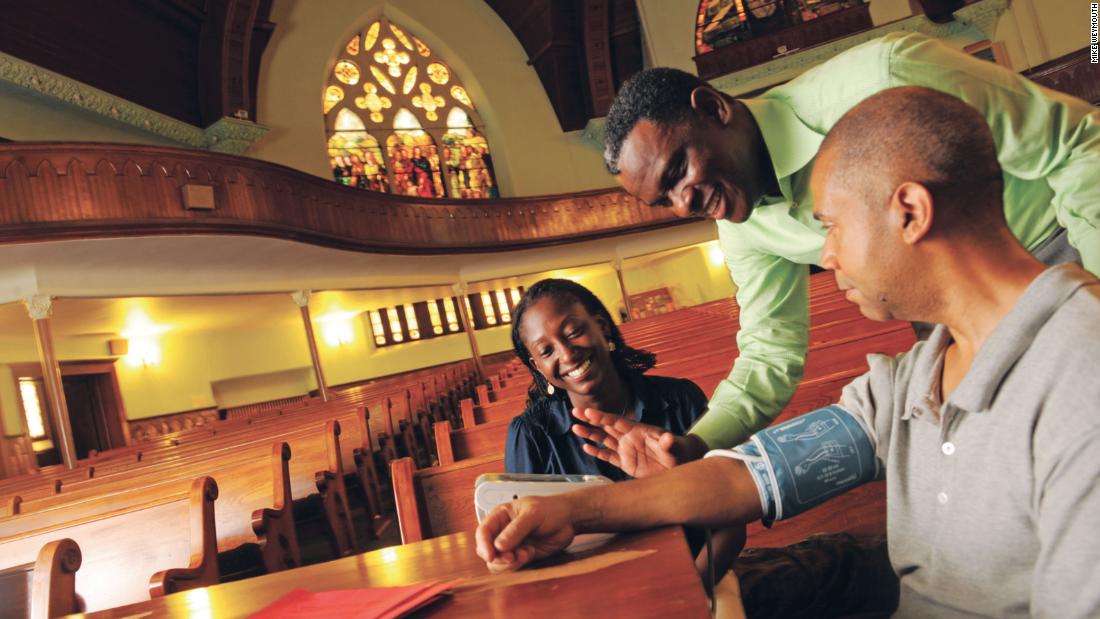
How church communities can help lower African-Americans’ blood pressure
(CNN)Amanda Hoyte-Badu was unsure how she would be perceived by a group of people a lot older than her. In her role as a lay health adviser, she was leading a session of mostly over-60-years-olds at Nazarene Congregational United Church of Christ in Brooklyn, New York.
“It turned out to be totally fine,” said Hoyte-Badu, who was 24 when she participated in the program. “They just appreciated having someone really listen to them and be understanding and nonjudgmental.”
Her leadership role was part of a new study of faith-based approaches in the treatment of hypertension in the black community; the results were published Tuesday in Circulation: Cardiovascular Quality and Outcomes Journal.
The researchers found that people who received therapeutic lifestyle advice and motivational interviewing sessions in a church environment had a greater reduction in systolic blood pressure levels than those who received only health education in churches.
“What we found was that for the group that had the intervention, there was a significantly lower blood pressure reduction in them than the other group. In other words, that group had a reduction in blood pressure by almost 6 points compared to the control group,” said Dr. Olugbenga Ogedegbe, an author of the study and professor and director in the Division of Heath and Behavior in the Department of Population Health at NYU Langone Medical Center.
Blood pressure is measured in two parts: systolic and diastolic. Systolic is the pressure when your heart is beating, and diastolic is the pressure when it’s resting, according to the US Centers for Disease Control and Prevention. A healthy blood pressure reading is less than 120/80 millimeters of mercury (noted as mmHg), with the first number systolic and the second diastolic. High blood pressure is 140/90 or higher.
The American Heart Association says nearly half of all non-Hispanic black adults in the United States have some form of cardiovascular disease. According to the American College of Cardiology’s Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults, 45.6% of American adults have hypertension.
For the new study, researchers split 373 people from 32 New York City churches into two groups. One, called the MINT-TLC group, attended 11 90-minute weekly group sessions focused on making healthy lifestyle changes. The sessions were run by members of the church acting as lay health advisers. These were followed up with three monthly phone calls updating one of the group leaders from the weekly sessions about their progress.
The other group received one lifestyle session focused on high blood pressure, also known as hypertension, and 10 sessions given by health experts on another topic such as Alzheimer’s disease or fire safety. Members of this group did not receive motivational calls.
Both groups had their blood pressure measured at the start of the program, six months after it began and nine months from the start.
The MINT-TLC group had a systolic blood pressure reduction of 16.53 mmHg after six months; members of the health education group had a systolic blood pressure reduction of 10.74. This culminated in a net reduction of 5.8 mmHg. The MINT-TLC drop had shrunk to 5.3 by nine months, but this was still clinically significant, according to Ogedegbe, who is also director of NYU Langone’s Center for Healthful Behavior Change.
Hoyte-Badu’s church was one of the first to become involved in the project.
She said she wanted to bring the project there because of the prevalence of high blood pressure and her own experience with family members who had hypertension.
“I thought it would be great to work with a program that would help people dealing with the condition lower their high blood pressure and just give them skills to help their health overall,” she said.
In her role as a health adviser, Hoyte-Badu was trained to lead sessions on topics such as how to lower blood pressure and set goals to improve health. She and two other advisers from her church also followed up with participants in the months after the intervention.
“The curriculum encouraged more dialogue and collaboration as opposed to us just lecturing to them, and I think they appreciate that, us being more collaborators as opposed to just teachers,” Hoyte-Badu said. “I think it created a safe environment and supportive environment for them to kind of share how they were doing with the challenges and just feel comfortable to share their journey in trying to make behavioral changes, because that’s really difficult.”
The sessions were always opened with a prayer by a health adviser or a participant, including Scripture that was relevant to that week’s topic, Hoyte-Badu said.
Members of her church received the project well and were excited to be a part of it, she said. At the end of the program, they had a potluck meal, and everyone bought a healthy dish they had learned about or had found themselves.
“The lay health model was a good one to have as part of the design,” said Mimi Kiser, a research assistant professor at Emory University’s Rollins School of Public Health, who was not involved in the study. “It fits well into the culture of the church and also into effective community-based strategies.”
She also said the study contributes to a gap in the literature around whether faith-based intervention projects are effective.
The use of the church as a location is significant to Kiser, who is also a senior program director at the Interfaith Health Program at Emory, especially in a community that may not have a trusting relationship with health care.
“Faith-based settings, they do tend to be sources of trusted information, and so when public health can align with those sources of trust in community-based efforts, it strengthens disease prevention and health promotion activities,” she said.
Sign up here to get The Results Are In with Dr. Sanjay Gupta every Tuesday from the CNN Health team.
Dr. Joseph Ravenell, associate professor of population health and medicine at the New York University School of Medicine, also saw the benefit of the lay health advisers. Although recent successful community-based methods have used counselors with doctorates and have focused on medication, Ogedegbe’s study emphasizes the need for other approaches.
The study “supports the notion that non-clinicians based in the community can be effective messengers for healthful behavior change in blacks with high blood pressure,” said Ravenell, who was not involved in the new research.
A study published in the New England Journal of Medicine in April found that placing health educators in barbershops in Los Angeles led to 63.6% of participants lowering their blood pressure to a healthy level. This showed how the combination of health promotion by community figures such as the barbers, combined with the use of medication, could have health benefits.
Ravenell also praised the latest study for its setting and its focus on the need for lifestyle changes in black adults with high blood pressure, which he described as “an important cornerstone of therapy for high blood pressure that is both underappreciated and under-studied in black populations.”




